VARIABILITY OF LENGTH OF THERAPY FOR POSSIBLE EARLY ONSET SEPSIS(EOS) AND LATE ONSET SEPSIS(LOS): IDENTIFYING OPPORTUNITIES FOR ANTIBIOTIC STEWARDSHIP IN THE NEONATAL INTENSIVE CARE UNIT(NICU)
I. Kopsidas, E. Bouza, T. Gouvias, A. Kaffe, K. Karachristou, E. Kourkouni, G. Mavrogeorgos, E. Roilides, T. Siahanidou, V. Soubasi, N. Spyridis, E. Stratiki, M. Theodoraki, P. Triantafyllidou, A. Tsintoni, G. Tsopela, M. Tzaki, T. Zaoutis
36th Annual Meeting of the European Society for Paediatric Infectious Diseases (ESPID 2018)
Malmö, Sweeden, May 28- June 2, 2018
BACKGROUND: Antibiotic resistance is a global public health threat and is associated with increased morbidity, mortality and healthcare costs. Antimicrobial stewardship is considered a core action in reducing antimicrobial resistance and is being advocated by all major health organizations globally. We sought to describe prescribing patterns in neonates treated for possible EOS and LOS and negative cultures.
METHODS: 15 public NICUs participated (September 2016-June 2017) and captured demographic, clinical, laboratory and antibiotic use data. The first 15 antibiotic initiations for unique patients were recorded each month. Cases with negative cultures were selected. Length of therapy (LOT) was calculated for each unit and described by median and IQR. Antibiotic consumption was measured for the first 7 days of each episode of EOS or LOS. Possible EOS was defined as one occurring within the first 2 days of life.
RESULTS: 1330 cases of possible EOS were recorded with a median LOT of 7 days(IQR:5-7.5). Median LOT, at the unit with the lowest value, was 3 days(IQR:2-4) while at the one with the highest 11(IQR:9-15). 260 cases of possible LOS were identified with a median LOT of 7 days (IQR:5-7.5). Median LOT, at the unit with the lowest value, was 4 days (IQR2-5) while at the one with the highest 10(IQR6-13). Median antibiotic consumption was: a)glycopeptides 2.7%(range:0-12.6%) for EOS and 21.7%(range:8.8%-34.8%) for LOS. b)meropenem 0.4%(range:0-4.8%)(EOS) and 8.6%(range:0-16.8%)(LOS), c)cefotaxime 1.2%(range:0%-12.5%)(EOS) and 2.2%(range:0-26.8%)(LOS)
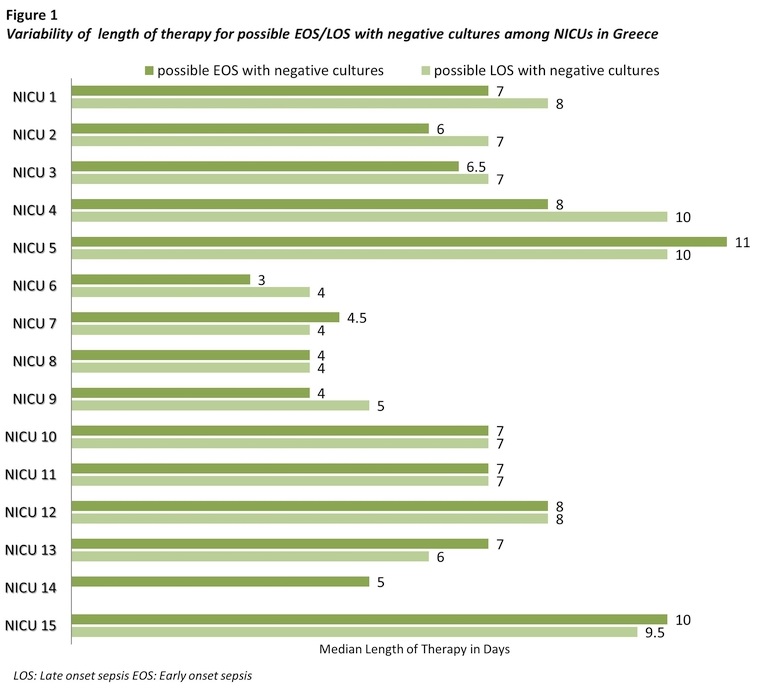
CONCLUSIONS: Benchmarking data on the variability of antibiotic use for common neonatal and pediatric indications is critical in identifying targets for antibiotic stewardship. We identified significant variability in the duration of therapy for EOS and LOS in the NICU. We are currently utilizing these data to design an intervention to improve antibiotic use in the NICUs nationally.



